Hernias are common, affecting about 5% of the population. A hernia occurs when an organ or fatty tissue protrudes through a weakened muscle wall or the fascia. Hernias most commonly occur in the abdomen, inner groin, outer groin, and umbilical areas. And, although they aren’t life threatening, they can become recurrent and unfortunately, hernias do not go away on their own. Within recent years, the use of meshes have become standard procedure in hernia repair surgeries around the world, and while this surgery is thought to reduce recurrences, there have been a number of complications which go along with the surgery, including mesh migration, mesh related infections, and chronic abdominal pain.
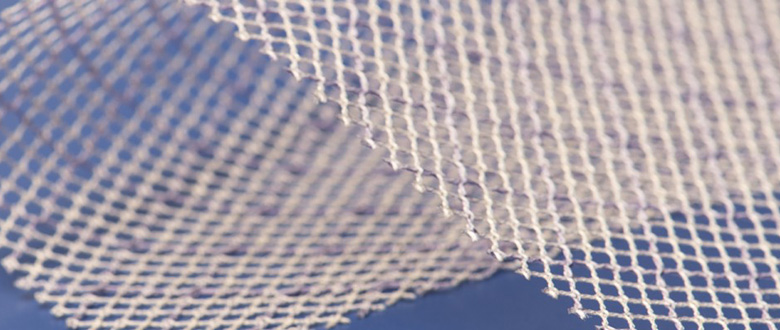
The use of surgical mesh for the treatment of hernias has drastically increased since the 1980’s, and by the year 2000, non-mesh repairs represented less than 10% of groin hernia repair techniques. Surgical meshes are typically constructed by synthetic materials or animal tissues. The synthetic type mesh comes in both knitted and non-knitted sheets, and can be made from either absorbable, or nonabsorbable materials. Animal-derived meshes are typically made from cow or pig intestines or skin, and then processed and disinfected to be used as an implantable device. Nonabsorbable mesh will remain in the body as a permanent implant, while absorbable implants tend to degrade and lose strength over time. It is thought that as the mesh degrades, new tissue will grow, providing strength to the repair. Some doctors use cheaper, polypropelene meshes because they are cheap and readily available. Unfortunately, this type of mesh can cause intense scarring and later issues.
According to the FDA, the most common adverse events after hernia mesh surgery are pain, infection, adhesions (scar-like tissue which sticks together), intestinal blockage, abnormal internal bleeding, or abnormal connections between organs and vessels. Along with these findings, there has been proof that recurrence after operation is most common, and typically caused by improper surgical techniques, migration of the mesh, or shrinkage of the mesh implant. Unfortunately, subsequent hernia operations in the same location are more challenging and prone to failure.
It is also understood that complications may increase over time. In one case, a lady was seen fourteen years after her surgery, complaining about intense abdominal pains. She complained about nausea, and bloating, as well as issues having bowel movements. After a CT scan came back unremarkable, it was found that the mesh had eroded into her lumen, and a two-stage operation would need to be done. According to a study in JAMA Surgery and presented at the 2016 Clinical Congress of American College of Surgeons, it was stated that the rate of complications increased after a five year period. “Out of the 3,242 study participants, 1,050 required subsequent abdominal surgery. Major complications included bowel obstruction, perforation and bleeding. Other serious complications included pain, non-healing wounds, infections, fluid buildup and organs fused together (fitulas). Larger pieces of mesh increased the risk of complications.”
Infections after hernia mesh surgery are also something to consider. Although the mesh is designed to be implanted, your body recognizes it as a foreign object, and the body naturally attempts to reject it, which increases the chance of infection of the tissues surrounding the mesh implant. Some of these infections can successfully be treated with antibiotics, but others, unfortunately have to have the mesh removed and find another solution for the hernia. In a long-term respective study of hernia mesh surgeries done is in Europe, the incidence of recurrence after a simple repair was still over 30%. They also found that complications due to the foreign body reaction causes postoperative seromas, hematomas, organ failure, mesh rejection, and fistula formation.
As mentioned above, there is also a chance of mesh migration, although, this tends to be a little more rare. Migration typically occurs when mesh is inadequately secured, or displaced by external forces. Secondary migration can also be triggered by foreign body reaction. In some cases, the mesh has migrated into the bladder, scrotum, or cecum. Surgeons have worked for years attempting to find a mesh that is more compatible, testing many different materials, pore sizes, weights, strengths, and biocompatibility.
Systematic bulging and chronic abdominal pain is also a factor after a hernia mesh surgery. Surgery mesh comes in different pore sizes, depending on the size of the hernia, and also the activity level of the patient. The mesh is exposed to stress under changes to intra-abdominal pressure. The mesh undergoes greater stress when a person coughs, jumps, or even vomits. The elasticity of the mesh should correspond to the elasticity of the abdominal wall, however, biomechanical studies have proven low stretch properties in these meshes, and bulging mesh is an important adverse effect which arises after surgery. Incidences in this systematic bulging vary from 1.6% to 17.4%. The inflammation caused by the bulging is known to cause chronic abdominal pain for patients, and according to Dr. Towfigh, of the Beverly Hills Hernia Center, 20% of patients will have post-operative pain for longer than three months, leading to loss of work, depression, and also opioid abuse. Dr. Towfigh has found that the groin and pelvis regions don’t seem to tolerate the mesh implant as well as areas of the abdominal region.
It is important to research and understand what complications can occur when considering a hernia mesh surgery. There are many meshes which have been recalled and removed from the market, and there are many lawsuits currently in effect over adverse reactions to hernia mesh surgeries.
Did You Suffer After a Hernia Mesh Operation?
If you suffered health problems after undergoing a hernia mesh procedure, then you may qualify for compensation. You may also qualify if you underwent a second surgery to correct a recurring hernia. Recovery may include past and future medical bills, lost wages, diminished quality of life, and pain and suffering.